Introduction:
Primary ovarian insufficiency (POI) is a well-documented late effect of cancer survivors that increases risk for primary or secondary amenorrhea, osteoporosis, cardiovascular disease, vasomotor symptoms, infertility, urogenital atrophy, cognitive decline, and overall increased mortality. There is limited data on the existing management and follow up of POI among female patients exposed to cancer treatments. The purpose of this study was to describe outcomes and management of POI in childhood leukemia and lymphoma survivors and patients with non-malignant hematological conditions treated with hematopoietic stem cell transplant (HSCT) at Children's Medical Center (CMC) in Dallas, Texas.
Methods:
A retrospective analysis was performed for 26 female patients identified through electronic survivorship database containing about 1200 records of female survivors followed at the CMC long-term follow-up (LTFU) program. Inclusion criteria were female patients diagnosed with a hematological malignancy or underwent HSCT due to a benign hematological condition, less than 18 years old at the time of diagnosis, and documented POI as a late effect. Moreover, ICD-9 codes for ovarian dysfunction, amenorrhea, oligomenorrhea, delayed puberty, and infertility were used to identify additional patients.
Results:
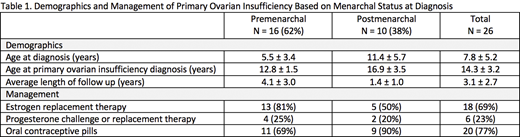
The mean age of the cohort was 7.8 ± 5.2 years at hematological diagnosis. Fifty-four percent of patients were leukemia survivors and 23% had lymphoma. Benign hematological conditions requiring HSCT were aplastic anemia (n = 2), sickle cell disease (n = 1), hemophagocytic lymphohistiocytosis (n = 1), macrophage activation syndrome (n = 1), and thrombocytopenia-absent radius syndrome (n = 1). Almost all survivors (24/26) were HSCT recipients; one patient received two HSCTs. Average age at diagnosis of POI was 14.3 ± 3.2 years with average follow-up of 3.1 ± 2.7 years.
At the time of POI diagnosis, 62% of survivors (16/26) were premenarchal. Average cyclophosphamide equivalent dose was 9.8 g/m2 for premenarchal and 13.8 g/m2 for postmenarchal females. In addition, 44% (7/16) of premenarchal compared to 50% (5/10) of postmenarchal female patients received either abdominopelvic or total body radiation.
Thirteen out of 16 premenarchal females received estrogen replacement therapy (ERT; 10 oral, 3 transdermal; Table 1). The other 3 patients achieved spontaneous menarche; one was initiated on oral contraceptive pills (OCPs) subsequently. Five premenarchal patients were monitored for growth or pubertal progression prior to initiating treatment; one was monitored due to improving gonadotropins. In 9 out of 10 premenarchal patients prescribed oral ERT, the dose was increased until vaginal spotting occurred. All patients that developed vaginal spotting while on ERT were eventually transitioned to OCPs. Four patients received progesterone challenge or combined replacement therapy prior to transition from ERT to OCPs.
Five out of 10 postmenarchal patients received oral ERT; all were eventually treated with OCPs, either after oral ERT or as initial treatment, except for one patient that was lost to follow-up. Two patients were treated with progesterone as challenge or combined replacement therapy but both received ERT previously and OCPs subsequently. Eight out of 10 postmenarchal patients resumed menses after POI treatment; the other two patients were not taking prescribed ERT or OCPs regularly.
Conclusions:
About 2% of females in our LTFU program were identified to have POI as a late effect, which is lower than reported in the literature, possibly due to younger age in our cohort. Almost all patients with POI were HSCT survivors. Our study shows that management of POI consists primarily of oral ERT with transition to OCPs and achieves resultant menarche in premenarchal female patients. Some premenarchal patients are monitored for growth and pubertal progression prior to treatment. In postmenarchal patients, treatment consists of OCPs that is sometimes preceded by ERT and leads to resolution of amenorrhea. Although OCPs demonstrated short-term benefit, perhaps replacement therapy at physiologic doses that imitate normal ovarian function more closely would have improved long-term outcomes. Additional studies are needed to investigate differences between hormone replacement therapy and OCPs and to identify the optimal approach in treating POI in cancer and HSCT survivors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal